- This event has passed.
2023 Annual Texas NMDOH Consortium Conference: Advancing Research, Policy and Practice
December 8, 2023 @ 8:30 am to 6:00 pm
The Texas Consortium for the Non-Medical Drivers of Health hosted its first Annual Conference. As US health expenditures continue to climb, investment by health system organizations in non-medical drivers of health presents an opportunity to increase the value of the dollars spent on health. This conference covered a range of topics related to advancing the research, policy, and practice of NMDOH in health care in Texas. NMDOH program sponsors, researchers, and funders/payers shared their expertise with conference attendees.
This event has passed, please click the following links to view presentation slides:
- Laura Gottlieb, MD – National Perspective on the Field of NMDOH
- Cecilia Ganduglia, MD – Medical Data + NMDOH Data
- Building Evaluation into NMDOH Programs from the Outset
- So You’ve Screened Your Patients–Now What?
- Building Your Team with a Medical-Legal Partnership
- Emily Sentilles – What You Need to Know about HHSC’s NMDOH Action Plan
- Crystal Ball: CMS next Steps on NMDOH
Session Times and Titles
*Agenda is approximate and subject to change
2023 Texas NMDOH Consortium Conference Speakers

Dr. Aliya Hussaini, Portfolio Director in Health, Michael & Susan Dell Foundation
Financing the Integration of NMDOH into Health Care Delivery
Aliya is responsible for the foundation’s efforts to improve health and wellness through proven strategies and partnerships with a broad range of traditional and non-traditional partners. She focuses primarily on improving health equity through addressing social drivers of health. Also core to her work is the management of the foundation’s investments in the Central Texas medical community.
Aliya completed undergraduate degrees in biology and economics at Swarthmore College, medical school at the University of Illinois at Chicago, pediatrics residency and chief residency at Yale New Haven Children’s Hospital, and fellowship training as a Robert Wood Johnson Clinical Scholar at the University of Pennsylvania, where she also earned a master’s degree in Health Policy Research. In addition to her work at the foundation, Aliya is a practicing pediatrician at People’s Community Clinic in Austin.

Brian Greene, President/CEO, Houston Food Bank
What’s Next? The Future of NMDOH in Texas
Brian Greene is President and CEO of the Houston Food Bank, a non-profit organization that uses donated food to better lives through a network of 1600 partnerships in 18 southeast Texas counties. Since taking the top post at the Houston Food Bank in 2005, Brian has led the organization to a fivefold increase in distribution. Houston Food Bank is now the largest food bank in the world and distributes more than two hundred million dollars of food each year to one million recipients. In 2021 Nonprofit Times named Brian one of the 50 most influential nonprofit leaders in the US.
Prior to moving to Houston, Brian was the Executive Director of the Second Harvest Food Bank of Greater New Orleans and Acadiana for 12 years. Previously, he held the same position at the Second Harvest Food Bank in Knoxville, Tennessee for 5 years. Brian is also an adjunct professor for the graduate program in Nonprofit Management at University of Houston Downtown. Brian has an MA in Economics from The University of Tennessee and a BA in Economics from Humboldt State University.

Brittany Whittington, Director of Accountable Care Systems, Integral Care
So You’ve Screened Your Patients – Now What?
Brittany Whittington is the Director of Accountable Care Systems at Integral Care, the Local Mental Health Authority serving Travis County, TX. She oversees all Population Health activities, in addition to Certified Community Behavioral Health Clinic (CCBHC) and Directed Payment Program operations. In 2019, Brittany helped launch Population Health at Integral Care, using data analytics and population profiles to identify at-risk patients and provide targeted interventions. In her role, she routinely performs analyses to identify cost and utilization trends among individuals with serious mental illness served by Integral Care. Her Return-on-Investment reports have been featured by the National Council for its role in identifying decreased utilization of emergency services through implementation of a mental health option for 911 calls.

Carol Paret, Retired, Memorial Hermann Healthcare System
Financing the Integration of NMDOH into Health Care Delivery
Carol Paret serves as a board member for Harris Health System. Carol is the former Senior Vice President and Chief Community Health Officer at Memorial Hermann Healthcare System. Her career at Memorial Hermann spanned over 40 years. From School Based Health Centers to a 24/7 Community Nurse Triage Line, to improving park infrastructure and programming in underinsured neighborhoods; this work focused on identifying a need that is impacting health and closing that gap.

Dr. Cecilia Ganduglia Cazaban, Physician, Associate Professor, Co-Director of the Center for Health Care Data, UTHealth Houston School of Public Health
Medical Data + NMDOH Data: Oh, the Places You’ll Go!
Dr. Ganduglia Cazaban is a medical doctor and Professor at UTHealth Houston School of Public Health. She is a highly trained health services researcher with extensive experience in the use of large administrative datasets for the evaluation of health care delivery, geographic variation in care processes, quality of care, and outcomes related to maternal and child health, chronic disease, and cardiovascular disease. She currently serves as the co-director of the Center for Health Care Data (CHCD), which is the largest research-accessible data center in Texas. The CHCD securely houses national and Texas-based claims data, electronic health records data, and non-medical drivers of health. The Center has recently been named the All-Payor Claims Database for the state of Texas (HB2090 87th Legislative) which includes claims data for 80% of the Texas insured population.
Dr. Ganduglia Cazaban has authored numerous publications to evaluate the quality of care, geographic variation in care processes, non-medical health drivers, outcomes, and costs related to chronic disease as well as maternal and newborn care.

Dr. Chethan Bachireddy, Senior Vice President and Chief Health Officer, Harris Health System
Financing the Integration of NMDOH into Health Care Delivery
Chethan Bachireddy, MD, MSc, FACP, AAHIVS, is the Senior Vice President and Chief Health Officer for Harris Health System. Dr. Bachireddy leads population health efforts to improve outcomes and reduce inequities among the county’s most vulnerable residents. In particular, his work focuses on applying evidence-based practices and accelerating health equity through transformative partnerships with academic, business, community and government entities.
Dr. Bachireddy has more than a decade of progressive leadership experience in care delivery transformation. As a physician, he holds board certifications in internal medicine and addiction medicine, and is an HIV specialist. He has dedicated his career to improving care and advancing equity for marginalized populations including those with HIV, substance use disorders and justice involvement as well as veterans and low-income patients.

Dr. Christina Fok, JD, General Pediatrician, Assistant Professor of Pediatrics, McGovern Medical School
Building your Team with a Medical-Legal Partnership
Dr. Christina Fok, MD, JD, is a General Pediatrician with UT Physicians and an Assistant Professor of Pediatrics at McGovern Medical School. Dr. Fok has expertise in Health Care Consumer Advocacy, helping patients navigate the medical system and working with underserved populations throughout her legal and medical training. She completed her law degree at the University of Wisconsin Law School in 2008 and received her medical degree from The University of Wisconsin School of Medicine and Public Health in 2016. She then went on to complete her Pediatric Residency Training at University of Texas Health Science Center in Houston. Dr. Fok joined UT Physicians and McGovern Medical School in 2019 and has been involved with the implementation of the Medical-Legal Partnership and screening for social determinants of health at the General Pediatrics Primary Care clinic at the Texas Medical Center. She also serves in the division of Pediatric Population Health, serving as the Co-Chair of the Social Determinants of Health Workgroup from 2021-2023, and currently the Director of the Pediatric Medical-Legal Partnership. She has presented her work on social determinants of health and medical-legal partnership at national and regional conferences. She is also involved in clinical education of medical students and pediatric residents and also lectured on non-medical drivers of health and health-harming legal needs. Dr. Fok recently joined the board of the Texas Medical-Legal Partnership Coalition in May of 2023.

Dr. Daniel Potter, Senior Director of Research, Rice University’s Kinder Institute
Building Evaluation into NMDOH Programs from the Outset
Daniel Potter is the Senior Director of Research at the Kinder Institute for Urban Research at Rice University. In his role, Dr. Potter oversees the five research centers that comprise KIUR, including the development and build-out of three new research centers focused on housing and neighborhoods, community and public health, and economic mobility and inequality. Dr. Potter is leading the Houston Population Research Center at Kinder, which houses the Kinder Houston Area Survey, which is about to begin its 43rd year and is the longest running survey of a major metropolitan area in the country. Dr. Potter has authored journal articles, research reports/briefs, and book chapters. Dr. Potter earned his Ph.D. in sociology from the University of Virginia.

Elena Marks, JD, Senior Health Fellow, Rice University’s Baker Institute
Financing the Integration of NMDOH into Health Care Delivery
Elena M. Marks is a Senior Fellow in Health at Rice University’s Baker Institute for Public Policy. Her work centers on improving health outcomes for all Texans, with an emphasis on people with low incomes and members of marginalized groups. Her areas of expertise include health systems, the Affordable Care Act, access to health care, health disparities, health equity, and the nonmedical drivers of health. From 2014 – 2022, Ms. Marks served as the Founding President and CEO of the Episcopal Health Foundation, a $1.3 billion philanthropy dedicated to health equity in Texas. Under her leadership, the foundation awarded over $400 million to nonprofits and governmental entities working to improve health outcomes.
Ms. Marks’ previous professional experiences include serving as the Director of Health and Environmental Policy for the City of Houston; consulting in the health care industry with large systems and community-based providers; starting and directing a successful legal placement firm; and practicing trial and appellate law with major law firms.

Emily Sentilles, Deputy Associate Commissioner and NMDOH Action Plan Lead, Texas Health & Human Services Commission
What You Need to Know About HHSC’s NMDOH Action Plan
Emily Sentilles serves as the Deputy Associate Commissioner for Quality and Program Improvement in the Medicaid and CHIP Services division at the Health and Human Services Commission (HHSC). The Quality and Program Improvement team mission is to advance the quality of the health care delivery system for Texans. The Quality and Program Improvement division is responsible for the MCS Non-Medical Drivers of Health Action Plan.
Emily has worked in state government for 15 years, starting at the Legislative Budget Board before joining HHSC in 2015. She holds a master’s degree in public affairs from the LBJ School of Public Affairs at The University of Texas at Austin and a bachelor’s degree in history from Brown University.

Dr. Jennifer Small, Executive Vice President and Administrator of Ambulatory Care Services, Harris Health System
Housing is Health: The Intensive Work of Addressing Housing Needs
Dr. Small serves as the Executive Vice President of Ambulatory Care Services (ACS) at Harris Health System where she provides administrative oversight and strategic direction of its integrated network of outpatient services that includes health centers, specialty clinics, mobile health units and its award-winning Health Care for the Homeless Program. Additionally, Dr. Small oversees Harris Health’s patient nurse hotline, Referral Center, Virtual Care and Patient Appointment Center. Dr. Small has held various leadership roles within ACS since 2009, serving as both the administrative director and vice president of primary care and specialty services. Throughout her time at Harris Health, she has focused on expanding access to care to vulnerable communities, including leading the expansion of specialty services within our community-based health centers and the integration of telemedicine services within the ACS platform.
Dr. Small graduated from the University of Texas at Austin with a Bachelor’s and Master’s in Communication Sciences and Disorders. She then earned a Doctor of Audiology at the University of Florida-Gainesville and a Master’s of Business Administration from the University of Houston-Bauer College of Business. She is a member of several professional and community organizations and serves on the boards of National Association of Health Services Executives-Houston and CollegeCommunityCareer. She also devotes much of her time mentoring students to mid-management leaders as they navigate their career path.

Jessica Pugil, Founder & Principal, Working Partner, LLC
Building Evaluation into NMDOH Programs from the Outset
Jessica Pugil is a skilled empowerment evaluator, facilitator, and strategic planner with over 25 years of experience in evaluating large, complex, multi-stakeholder, multi-site initiatives. Over the years, she has performed evaluations in healthcare and public health, workforce development, and community development, and led multiple community-wide strategy initiatives in economic development and disaster recovery. Jessica holds a bachelor’s degree in political science from McGill University and a master’s degree in public affairs from the LBJ School of Public Affairs. A committed collaborator, she is an active participant of the Texas Evaluation Network and the American Evaluation Association.

Joel Hunt, Physician Assistant, JPS Health Network
Housing is Health: The Intensive Work of Addressing Housing Needs
Joel Hunt has over 15 years of delivering healthcare to marginalized people. He graduated from the University of Utah where he received a Masters of Physician Assistant Studies after serving 6 years in the US Army. Joel began his career in medicine with people experiencing homelessness in Salt Lake City, Utah at a Health Care for the Homeless grantee and Federally Qualified Health Clinic where he started a street medicine program. At JPS Health Network and Acclaim Physician Group he has been responsible for oversight and implementation of the street medicine team, collaborating with community partners for development of services such as integrating housing and health care, recuperative care, health care and homelessness research. Also integral are the broad training opportunities including fellowship and resident physician programs as well as in-depth student rotations in street medicine. Joel has co-authored peer reviewed articles and presented internationally about homelessness and street medicine. Joel’s goal is to bring healthcare to people experiencing homelessness, improve health outcomes, reduce suffering, and promote dignity and equity resulting in a positive community impact.

Dr. John Wesley McWhorter, Vice President, Lifestyle Medicine, Suvida Healthcare
Listen to the Experts: How to Overcome Blind Spots to Integrating Food is Medicine Programs
John “Wesley” McWhorter is a professional chef, registered dietitian, behavioral scientist, and food-as-medicine expert. Currently the Vice President of Lifestyle Medicine at Suvida Healthcare, he also serves as a national spokesperson for the Academy of Nutrition and Dietetics, an advisory council member for the Teaching Kitchen Collaborative, and a community board member for the American Diabetes Association. Dr. McWhorter is dedicated to advancing hands-on culinary medicine education and food-as-medicine programming, focusing on promoting nutrition equity. He frequently publishes academic and practice-oriented research, contributes to textbooks, and has authored an award-winning cookbook. Wesley previously served as an assistant professor at McGovern Medical School and the University of Texas School of Public Health, where he was also the Director of Culinary Nutrition for the Nourish Program. Wesley received his culinary training from the Florida Culinary Institute, his undergraduate degree from Kansas State University, his master’s degree from the University of Texas Medical Branch, and his doctorate in Health Promotion and Behavioral Science from the University of Texas Health Science Center School of Public Health in Houston, TX.

Jolene Rasmussen, Chief Strategy Officer, Texas Council of Community Centers
So You’ve Screened Your Patients – Now What?
Jolene K. Rasmussen, MS, the Chief Strategy Officer for the Texas Council of Community Centers leads statewide and system-wide behavioral health innovations promoting data-driven clinical and fiscal excellence. For over two decades Jolene has led transformative initiatives, such as CCHBC development, population health, 1115 Medicaid Waivers, alternative payment models, behavioral and physical health integration, MCO evaluation, and HEDIS measurement. Jolene blends her academic background in research, data analysis, epidemiology, and anthropology, with her decades working for a state association, a state government, and several premier research institutes; her talent is creating and analyzing powerful research and turning results into practical provider-level solutions. She thrives when collaborating with other creative innovators around the country.

Kayla Mize, Marketplace Coordinator, Waco Family Medicine
Building Evaluation into NMDOH Programs from the Outset
Kayla Mize, LMSW is the Marketplace Coordinator at Waco Family Medicine, where she oversees partnerships with community-based organizations to connect patients to services that address non-medical drivers of health. She previously coordinated Waco Family Medicine’s Medical-Legal Partnership with Greater Waco Legal Services, serving as a bridge between organizations, providing support to clinicians, attorneys, and other staff to ensure that patients’ health-harming legal needs were identified and addressed. Kayla graduated from Baylor University with her Bachelor’s in Social Work in 2012 and her Master’s in Social Work in 2014. Upon completion of her MSW, Kayla managed the Baylor undergraduate social work program until 2021, then became the Heart of Texas Regional Director with the Baylor Collaborative on Hunger and Poverty before joining Waco Family Medicine.

Keegan Warren, Executive Director, Texas A&M Institute on Healthcare Access
Building your Team with a Medical-Legal Partnership
Keegan Warren, JD, LLM, is the Executive Director of Texas A& M University’s new Institute on Healthcare Access. She brings lived experience and a civil justice lens to bear on health and wellness, specializing in non-medical cost drivers and health equity. An attorney and Federally Qualified Health Center director with nearly two decades of senior management experience spanning health and human services, she is a national expert on integrating medical and social services through medical-legal partnership, a care delivery model that leverages legal expertise to advance individual and population health. Warren’s research and writing focuses on integration of non-medical drivers of health, including identifying institutional policies that may be inadvertently worsening disparities and raising costs. She has significant experience helping stakeholders navigate confidentiality and privacy to facilitate patient-centered data-sharing across sectors. Her expertise includes policy surveillance on targeted access issues, with recent focus on treating opioid use disorder in carceral settings.

Kent McKeever, Founder, Greater Waco Legal Services
Building your Team with a Medical-Legal Partnership
Kent McKeever, JD, founded Greater Waco Legal Services in 2017 with a passion for providing folks in Waco-McLennan County and surrounding areas access to the justice system through affordable legal representation, advice and resources. Kent serves as the Managing Attorney Partner and works with clients on cases involving immigration, wills, probate, and property. Kent graduated from Baylor University in 2001 and Princeton Theological Seminary in 2004. While serving as a youth minister and Pastor/Director of a non-profit ministry, Kent saw the need for legal advocacy on many levels, which led him to Vanderbilt Law School (J.D. 2012). After law school, Kent started a legal services program with Mission Waco, and it laid the foundation for the realization of the dream of this nonprofit law firm. Kent is the proud husband of Emily and father of Zoe, CJ, and Mathis. His education degrees include a J.D. from Vanderbilt Law School in 2012, A Master’s of Divinity from Princeton Theological Seminary in 2004, and Bachelor’s from Baylor University in 2001.

Dr. Laura Gottlieb, Professor and Founding Director of Social Integration Research and Evaluation Network (SIREN), University of California San Francisco
National Perspective on the Field of NMDOH
Dr. Gottlieb is a Professor of Family and Community Medicine at the University of California, San Francisco. Her research explores health care sector programs and policies related to identifying and addressing social risk factors in the context of care delivery. She is the founding co-director of the Social Interventions Research and Evaluation Network, a national research network that advances research on health care strategies to improve social conditions. Dr. Gottlieb is also Associate Director of the Robert Wood Johnson Foundation Evidence for Action National Program Office.

Dr. Leslie Wainwright, Chief Funding and Innovation Officer, Parkland Center for Clinical Innovations
Texas NMDOH Consortium Crystal Ball: CMS Next Steps on NMDOH
Leslie Wainwright is chief funding and innovation officer, Parkland Center for Clinical Innovations, Dallas. Her experience includes academic research, pharma/biotechnology and healthcare delivery; working with startups and multinational executive teams in creating growth strategies and alternative business models; and evaluating emerging clinical\care delivery technologies. Dr. Wainwright speaks on future of healthcare, enabling technologies, disruptive innovation and emerging business models. Prior to joining Parkland, she oversaw RTI International’s Innovation Advisors health practice, guiding the development and adoption of healthcare innovation. She has held executive roles with Sg2, AVIA and Business Models Inc. Dr. Wainwright earned her doctorate in microbiology at Northwestern University, and completed postdoctoral research training at the University of Maryland’s Center for Vaccine Development.

Dr. Maninder Kahlon, Vice Dean of Health Ecosystem, Director of Factor Health, Dell Medical School
Listen to the Experts: How to Overcome Blind Spots to Integrating Food is Medicine Programs
“Maninder “Mini” Kahlon is the founder of Factor Health, an incubator for programs that deliver clinically-relevant results by influencing the factors that affect health in our lives. Solutions address diabetes, kidney health, maternal health, depression, and loneliness, incorporating innovations in the workforce, nutritional and behavioral science, and payment design. A key goal is to move the system to pay for non-medical drivers, including food as medicine, with trials that test the impact of food within person-centered programs to influence clinically-relevant outcomes of health.
Mini is a founding Vice Dean at the recently launched Dell Medical School at the University of Texas at Austin and an associate professor in the Department of Population Health. Prior to this, she managed the nation’s largest translational science institute at UCSF and has led the development of award-winning collaborative and networking technologies in industry and academic medicine. Current advisory roles include Mini contributes to health transformation locally and nationally, including as founding Co-Chair of Austin Healthcare Council, Steering Committee for Food as Medicine, Texas NMDOH Consortium and as Advisory Board member for CaroNova, a health transformation initiative of the healthcare associations of North & South Carolina. She received her Ph.D. in neuroscience from the University of California, San Francisco (UCSF).”

Marisa Luera, Director, Sellers Dorsey LLC
Financing the Integration of NMDOH into Health Care Delivery
Marisa has an established reputation in Texas Medicaid with over 20 years professional experience. She is a health care policy professional providing strategic guidance, technical expertise, and stakeholder engagement to managed care plans, government entities, and solution partners. Prior to joining Sellers Dorsey, Marisa served the Texas Health and Human Services Commission in Medicaid and CHIP Program Policy and led key program policy and development initiatives. Marisa also has state and federal legislative experience and spent the first part of her career working in the nonprofit sector. Marisa received her undergraduate degree from Texas A&M University and her master’s degree from Columbia University.

Michelle Murdock, Vice President of Operations, Long Term Services & Supports, Superior HealthPlan
Housing is Health: The Intensive Work of Addressing Housing Needs
Michelle Murdock is the Vice President of Operations for Long Term Services & Supports (LTSS) for Superior HealthPlan, Centene Corporation’s Texas-based healthcare organization. Murdock and her colleagues administer Medicaid and Managed LTSS (MLTSS) programs in Texas, serving approximately 2 million across all 254 counties in the state.
Overall, she has 25 years of healthcare experience, primarily focused on serving vulnerable Medicaid populations. Murdock has also served as a Peace Corps Volunteer, supporting marginalized urban communities and at-risk youth.

Rosie Valadez-McStay, Founder and Strategic Consultant, RVM Strategies LLC
What’s Next? The Future of NMDOH in Texas
Rosie Valadez McStay, MPH, has over 25 years of health policy and healthcare administration experience, especially in Medicaid, CHIP, managed care, and community health. As the former executive of Government Relations and Community Benefits for one of the nation’s top five children’s hospitals, Ms. Valadez McStay worked with colleagues locally, across Texas, and the nation to improve the health and well-being of families through public policy and community health advocacy. Through her leadership and her team’s efforts, Ms. Valadez McStay championed legislation that expanded Medicaid coverage for children and pregnant women, the passage of the Children’s Health Insurance Program in Texas, national policies to fund pediatric graduate medical residency programs, and federal policies to improve care coordination for medically complex children in Medicaid and CHIP.
Ms. Valadez McStay guided the hospital’s inaugural 1115 Medicaid waiver incentive payment program and coordinated numerous community health needs assessments and community benefit implementation plans for the children’s health system. Examples of her successful advocacy include securing over $100 million in CARES funding, partnering with the city and county public health systems to provide COVID-19 health care information to immigrant and disenfranchised families, and basic resources to neighbors disproportionately impacted by the pandemic. She is passionate about health equity and collaboration on prevention strategies that improve overall community health and well-being. She holds a Bachelor of Liberal Arts in American Studies from the University of Texas at Austin and earned her Masters in Public Health from UT Health – Houston.

Dr. Shao-Chee Sim, Vice President for Research, Innovation and Evaluation, Episcopal Health Foundation
What’s Next? The Future of NMDOH in Texas
Shao-Chee Sim has been the Episcopal Health Foundation’s Vice President for Research, Innovation and Evaluation since 2015. Sim is also a nonresident fellow in health policy at Rice University’s Baker Institute for Public Policy, where his work focuses on health policy and social determinants of health research. He currently leads the Foundation’s work in health coverage and health policy analysis; pilot projects, learning collaboratives; research and evaluation portfolio. Current priorities include Medicaid managed care organizations social determinants of health (SDOH) strategies, multi-sectoral community health collaboratives, innovative SDOH financing strategies, community health center payment reform, rural healthcare service delivery, and public opinion survey research.
He earned his Master’s degree in public administration from the JFK School of Government at Harvard University and a doctorate in public policy from the LBJ School of Public Affairs at the University of Texas at Austin.

Shannon Ghangurde, Budget and Legislative Consultant, Shannon Ghangurde Consulting
What’s Next? The Future of NMDOH in Texas
Shannon Ghangurde has nearly two decades of legislative and state budget experience working in the Texas Legislature. Prior to starting her own consulting practice, Shannon served as the Committee Director for the Senate Finance Committee where she oversaw the budget writing process for all areas of state government, including health care, education, transportation, natural resources and general government services. During her time at the Capitol, she also served as the Committee Director for the Senate Health and Human Services Committee and General Counsel to Texas Senator Jane Nelson, where she helped lead negotiations on marquee initiatives including the health care portion of the state budget, Medicaid reform, historic advances for mental health, and the creation of the nation’s largest cancer research institute, CPRIT.
Shannon holds a B.A. degree in government from the University of Texas at Austin and a law degree from the Washington College of Law at American University. A native Texan, Shannon resides in Austin with her husband and two children, who enjoy traveling and the outdoors.

Sharon Grady, Attorney, Texas RioGrande Legal Aid
Building your Team with a Medical-Legal Partnership
Sharon Grady, JD, is an attorney with Texas RioGrande Legal Aid (TRLA) based out of San Antonio, Texas. She is the primary advocate in the inaugural Medical Legal Partnership between TRLA and Methodist Healthcare Ministries. Before practicing law, Ms. Grady was a Coordinator for Education Service Center Region 20, where she implemented a Head Start program via an integrated partnership model across four local school districts. Additionally, Ms. Grady has over a decade of experience as a Licensed Child Placing Agency Administrator working in the foster care system. She has two nieces and two dogs that keep her busy and fill her heart.

Dr. Shreela Sharma, Professor, Director of Center for Health Equity, UT Houston School of Public Health
Listen to the Experts: How to Overcome Blind Spots to Integrating Food is Medicine Programs
Shreela Sharma, PhD, RDN is the founding Director of the Center for Health Equity. She is also Professor & Vice Chair of the Department of Epidemiology at UTHealth Houston School of Public Health. As a trained dietitian and physical therapist, she realized she was treating diseases stemming from poor lifestyles: heart disease, diabetes, and hypertension. Sharma completed her PhD in epidemiology with a minor in biostatistics, health promotion, and behavioral sciences to address the systemic inequities leading to high rates of preventable disease and their devastating repercussions in the community. Her research interests are in health equity, health disparities, and behavioral epidemiology with a focus on food insecurity, diet quality, and chronic disease prevention among low-income, ethnically diverse families and communities using a policy, systems, and environment approach. Sharma is committed to the community. She co-leads the Health Equity Collective, a systems coalition in the Greater Houston region with a singular mission of care coordination for social determinants of health needs using a collective impact approach. She also co-founded Brighter Bites, a nationwide non-profit dedicated to providing fresh produce and nutrition education to low-income children and their families.

Dr. Steve Miff, President & CEO, Parkland Center for Clinical Innovations
Texas NMDOH Consortium Crystal Ball: CMS Next Steps on NMDOH
Dr. Miff is the President and CEO of Parkland Center for Clinical Innovation (PCCI), a leading, non-profit, artificial intelligence and cognitive computing organization affiliated with Parkland Health, one of the country’s largest and most progressive safety-net hospitals. Spurred by his passion to use next-generation analytics and technology to help serve the most vulnerable and underserved residents, Steve and his team focus on leveraging technology, data science, and clinical expertise to obtain unique social-determinants-of-health data and incorporate those holistic, personal insights into point-of-care interventions.

Wayne Young, Chief Executive Officer, The Harris Center for Mental Health & IDD
Housing is Health: The Intensive Work of Addressing Housing Needs
As the Chief Executive Officer of one of the largest behavioral health organizations in the nation, Wayne Young is passionate about the planning and delivery of large-scale behavioral health and intellectual and developmental disabilities services to a population who rely upon safety net systems of care. Wayne previously served as the chair of the Texas Health and Human Services Commission’s Behavioral Health Advisory Council and was recently appointed by the Supreme Court of Texas to the Texas Judicial Commission on Mental Health. Wayne was honored to have received the Charley H. Shannon Advocate for Justice Award from NAMI Texas in 2019 as well as to have been named to Modern Healthcare’s list of Top 25 Innovators in 2019 and again 2021. In 2023, Wayne was recognized as one of Houston’s Most Admired CEO’s. While honored by individual recognitions, Wayne is most proud to have been a part of The Harris Center as it received the Excellence Award for Innovation from the National Council on Behavioral Health and was named as a Best Place to Work by The Houston Business Journal who also honored them with a Diversity in Business Award in 2023.

William Lyons, Sr. Manager of Programs for Health Connect, Legacy Community Health
Building Evaluation into NMDOH Programs from the Outset
William Lyons has served as Sr, Manager of Programs, Social Determinants of Health at Legacy Community Health since January 2019. He is a LCSW (advanced social work professional) and supervisor with over decade of experience across fields; including case management, clinical mental health services, community organizing, financial coaching, and non-profit management. Specific expertise includes trauma-informed care, motivational interviewing, and critical time intervention. In his current role at Legacy, he primarily supports the professional development of student interns as emerging healthcare professionals across disciplines. He serves on a few workgroups such as Community Voice with the Health Equity Collective, Accountable Community of Health of Greater Northside, and Coalition for Environment Equity & Resilience. In addition, he is a therapist providing services to youth (12 – 17) individually and a therapy group for Queer youth experiencing anxiety, depression, and gender dysphoria.

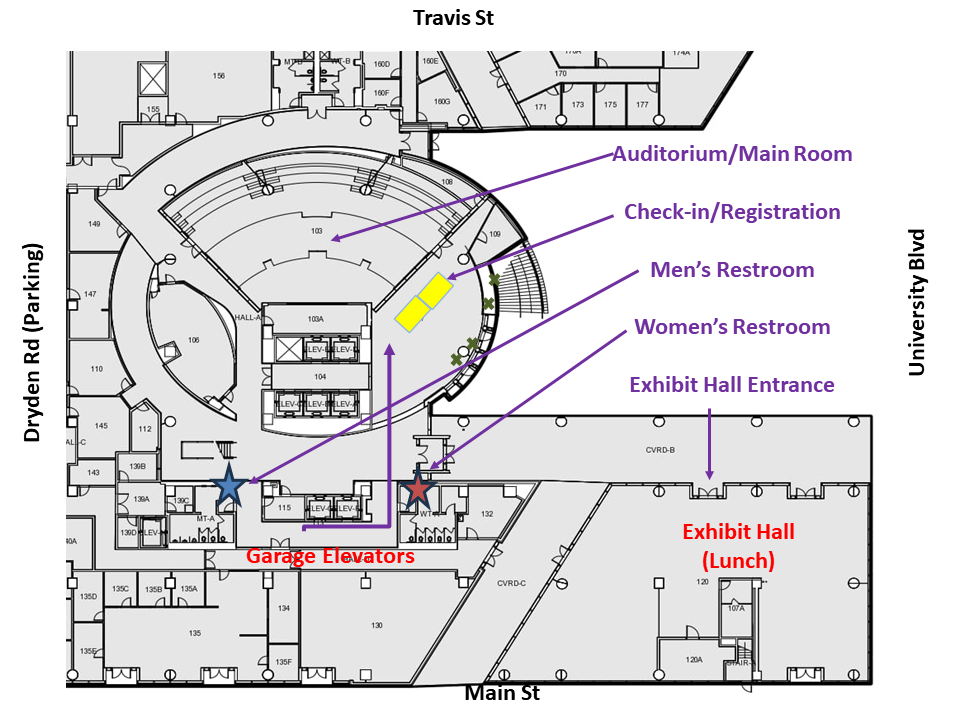
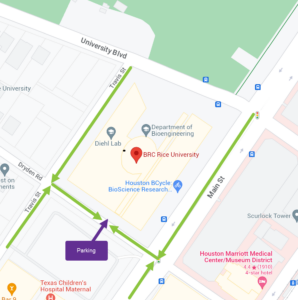
6580 Fannin Street
Houston, TX 77030
1709 Dryden Road
Houston, TX 77030
Parking validations will be provided upon check-in.